U.S. FDA Approves Supplemental New Drug Application (sNDA) for ERLEADA® (apalutamide) for the Treatment of Patients with Metastatic Castration-Sensitive Prostate Cancer (mCSPC)
Phase 3 TITAN is the first registrational study to achieve statistical significance in dual primary endpoints of overall survival and radiographic progression-free survival in patients with mCSPC regardless of extent of disease
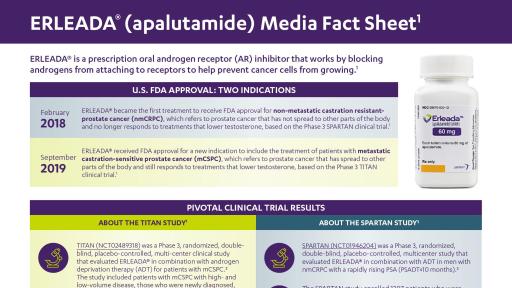
HORSHAM, Pa., September 17, 2019 – The Janssen Pharmaceutical Companies of Johnson & Johnson announced today that the U.S. Food and Drug Administration (FDA) has approved ERLEADA® (apalutamide) for the treatment of patients with metastatic castration-sensitive prostate cancer (mCSPC).1 Today’s approval follows FDA Priority Review Designation of the supplemental New Drug Application (sNDA) that was submitted in April 2019 and reviewed through the FDA Real-Time Oncology Review program. The new indication for ERLEADA® will make this androgen receptor inhibitor available for the approximately 40,000 people in the U.S. diagnosed with mCSPC annually.2
Approval is based on results from the Phase 3 TITAN study, which achieved statistical significance in the dual primary endpoints of overall survival (OS) and radiographic progression-free survival (rPFS) at the first pre-planned interim analysis.3 The trial recruited patients regardless of extent of disease, including both high- and low- volume disease, or prior docetaxel treatment history.1,3 Results were presented in an oral session at the 2019 American Society of Clinical Oncology (ASCO) Annual Meeting and simultaneously published in The New England Journal of Medicine.
“Prostate cancer is more difficult to treat once it spreads, and for patients with castration-sensitive disease, it is clear that androgen deprivation therapy (ADT) alone, is often not enough,” said Dr. Kim Chi, Medical Oncologist at BC Cancer - Vancouver and principal investigator of the TITAN study. “Results from the TITAN study showed that, regardless of the extent of disease, patients with metastatic castration-sensitive prostate cancer have the potential to benefit from treatment with apalutamide in addition to ADT.”
In the TITAN study, ERLEADA® plus ADT significantly extended OS compared to placebo plus ADT with a 33 percent reduction in the risk of death (HR=0.67; 95 percent CI, 0.51-0.89; P=0.0053).1 ERLEADA® plus ADT also significantly improved rPFS compared to placebo plus ADT with a 52 percent lower risk of radiographic progression or death (HR=0.48; 95 percent CI, 0.39-0.60; P<0.0001).1 As reported in the published results from the TITAN study, the two-year OS rates, after a median follow-up of 22.7 months, were 84 percent for ERLEADA® plus ADT compared to 78 percent for placebo plus ADT.3
“ERLEADA® has the potential to change how patients with prostate cancer are treated, regardless of the extent of the disease or prior docetaxel treatment history, by delaying disease progression and prolonging survival,” said Margaret Yu, M.D., Vice President, Prostate Cancer Disease Area Leader, Janssen Research & Development, LLC. “This milestone highlights Janssen’s commitment to improve the standard of care for patients with prostate cancer as we continue to develop innovative treatments across the disease continuum.”
The most common adverse reactions (≥10 percent) that occurred more frequently in ERLEADA® treated patients (≥2 percent over placebo) from the randomized placebo-controlled clinical trials (TITAN and SPARTAN) were fatigue, arthralgia, rash, decreased appetite, fall, weight decreased, hypertension, hot flush, diarrhea, and fracture.1
For the full U.S. Prescribing Information, please visit www.ERLEADA.com.
About the TITAN Study1
TITAN (NCT02489318) is a Phase 3, randomized, placebo-controlled, double-blind study in patients with mCSPC. The study included 1,052 patients in 23 countries across 260 sites in North America, Latin America, South America, Europe, and Asia Pacific. Patients with mCSPC were randomized 1:1 and received either ERLEADA® (240 mg) plus ADT (n=524), or placebo plus ADT (n=527). The recruitment period for the study spanned from December 2015 to July 2017.1 The study included patients with mCSPC with both low- and high-volume disease, and those who were newly diagnosed, or those who had received prior definitive local therapy or prior treatment with up to six cycles of docetaxel for mCSPC.3
An Independent Data-Monitoring Committee was commissioned by the sponsor to monitor safety and efficacy.3 Dual primary endpoints of the study were OS and rPFS.1 Secondary endpoints included time to cytotoxic chemotherapy, time to pain progression, time to chronic opioid use, and time to skeletal-related event.3 Exploratory endpoints included time to PSA progression, PFS2 and time to symptomatic progression.3 For additional study information, visit ClinicalTrials.gov.
About Metastatic Castration-Sensitive Prostate Cancer
Metastatic castration-sensitive prostate cancer (mCSPC), also known as metastatic hormone-sensitive prostate cancer (mHSPC), refers to prostate cancer that still responds to ADT and has spread to other parts of the body.4
About ERLEADA®
ERLEADA® (apalutamide) is an androgen receptor (AR) inhibitor indicated for the treatment of patients with non-metastatic castration-resistant prostate cancer (nmCRPC) and for the treatment of patients with mCSPC. ERLEADA® received FDA approval for nmCRPC on February 14, 2018 and was approved for mCSPC on September 17, 2019.1 ERLEADA® taken orally, once daily, with or without food.1 The NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for Prostate Cancer include apalutamide (ERLEADA®) as a treatment option for patients with non-metastatic (M0) CRPC with a Category 1 recommendation for those with a PSA doubling time ≤10 months.*5 The NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) include apalutamide (ERLEADA®) with androgen deprivation** as a Category 1 treatment option for patients with metastatic (M1) castration-naive prostate cancer.†5 The American Urological Association (AUA) Guidelines for Castration-Resistant Prostate Cancer (CRPC) recommend clinicians offer apalutamide (ERLEADA®) with continued androgen deprivation therapy (ADT) as one of the treatment options for patients with nmCRPC at high risk for developing metastatic disease. (Standard; Evidence Level Grade A)***.6 ERLEADA® is being studied in five Phase 3 clinical trials.
* Referenced with permission from the NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for Prostate Cancer V.4.2019. © National Comprehensive Cancer Network, Inc. 2019. All rights reserved. Accessed September 16, 2019. To view the most recent and complete version of the NCCN Guidelines®, go online to NCCN.org. NCCN makes no warranties of any kind whatsoever regarding their content, use, or application, and disclaims any responsibility for their application or use in any way.
** Orchiectomy, LHRH agonist, or LHRH antagonist
† The term “castration-naive” is used to define patients who are not on ADT at the time of progression. The NCCN Prostate Cancer Panel uses the term “castration-naive” even when patients have had neoadjuvant, concurrent, or adjuvant ADT as part of radiation therapy provided they have recovered testicular function.
***Standard: Directive statement that an action should (benefits outweigh risks/burdens) or should not (risks/burdens outweigh benefits) be taken based on Grade A or B evidence.
***Evidence Level: A designation indicating the certainty of the results as high, moderate, or low (A, B, or C, respectively) based on AUA nomenclature and methodology.
ERLEADA® IMPORTANT SAFETY INFORMATION1
WARNINGS AND PRECAUTIONS
Ischemic cardiovascular events — In a randomized study (SPARTAN) of patients with nmCRPC, ischemic cardiovascular events occurred in 4% of patients treated with ERLEADA® and 3% of patients treated with placebo. In a randomized study (TITAN) in patients with mCSPC, ischemic cardiovascular events occurred in 4% of patients treated with ERLEADA® and 2% of patients treated with placebo. Across the SPARTAN and TITAN studies, 6 patients (0.5%) treated with ERLEADA® and 2 patients (0.2%) treated with placebo died from an ischemic cardiovascular event. Patients with current evidence of unstable angina, myocardial infarction, or congestive heart failure within six months of randomization were excluded from the SPARTAN and TITAN studies.
Ischemic cardiovascular events, including events leading to death, occurred in patients receiving ERLEADA®. Monitor for signs and symptoms of ischemic heart disease. Optimize management of cardiovascular risk factors, such as hypertension, diabetes, or dyslipidemia. Consider discontinuation of ERLEADA® for Grade 3 and 4 events.
Fractures — In a randomized study (SPARTAN) of patients with nmCRPC, fractures occurred in 12% of patients treated with ERLEADA® and in 7% of patients treated with placebo. In a randomized study (TITAN) of patients with mCSPC, fractures occurred in 9% of patients treated with ERLEADA® and in 6% of patients treated with placebo. Evaluate patients for fracture risk. Monitor and manage patients at risk for fractures according to established treatment guidelines and consider use of bone targeted agents.
Falls — In a randomized study (SPARTAN), falls occurred in 16% of patients treated with ERLEADA® compared to 9% of patients treated with placebo. Falls were not associated with loss of consciousness or seizure. Falls occurred in patients receiving ERLEADA® with increased frequency in the elderly. Evaluate patients for fall risk.
Seizure — In two randomized studies (SPARTAN and TITAN), five patients (0.4%) treated with ERLEADA® and one patient treated with placebo (0.1%) experienced a seizure. Permanently discontinue ERLEADA® in patients who develop a seizure during treatment. It is unknown whether anti-epileptic medications will prevent seizures with ERLEADA®. Advise patients of the risk of developing a seizure while receiving ERLEADA® and of engaging in any activity where sudden loss of consciousness could cause harm to themselves or others.
Embryo-Fetal Toxicity — The safety and efficacy of ERLEADA® have not been established in females. Based on its mechanism of action, ERLEADA® can cause fetal harm and loss of pregnancy when administered to a pregnant female. Advise males with female partners of reproductive potential to use effective contraception during treatment and for 3 months after the last dose of ERLEADA® [see Use in Specific Populations (8.1, 8.3)].
ADVERSE REACTIONS
Adverse Reactions — The most common adverse reactions (≥10%) that occurred more frequently in the ERLEADA®-treated patients (≥ 2% over placebo) from the randomized placebo-controlled clinical trials (TITAN and SPARTAN) were fatigue, arthralgia, rash, decreased appetite, fall, weight decreased, hypertension, hot flush, diarrhea and fracture.
Laboratory Abnormalities — All Grades (Grade 3-4)
- Hematology — In TITAN study, white blood cell decreased ERLEADA® 27% (0.4%), placebo 19% (0.6%). In SPARTAN study anemia ERLEADA® 70% (0.4%), placebo 64% (0.5%); leukopenia ERLEADA® 47% (0.3%), placebo 29% (0%); lymphopenia ERLEADA® 41% (2%), placebo 21% (2%)
- Chemistry — In TITAN study, hypertriglyceridemia ERLEADA® 17% (3%), placebo 12% (2%). In SPARTAN study hypercholesterolemia ERLEADA® 76% (0.1%), placebo 46% (0%); hyperglycemia ERLEADA® 70% (2%), placebo 59% (1%); hypertriglyceridemia ERLEADA® 67% (2%), placebo 49% (0.8%); hyperkalemia ERLEADA® 32% (2%), placebo 22% (0.5%).
Rash — In two randomized studies, rash was most commonly described as macular or maculo-papular. Adverse reactions of rash were 26% with ERLEADA® versus 8% with placebo. Grade 3 rashes (defined as covering >30% body surface area [BSA]) were reported with ERLEADA® treatment (6%) versus placebo (0.5%). The onset of rash occurred at a median of 83 days. Rash resolved in 78% of patients within a median of 78 days from onset of rash. Rash was commonly managed with oral antihistamines, topical corticosteroids, and 19% of patients received systemic corticosteroids. Dose reduction or dose interruption occurred in 14% and 28% of patients, respectively. Of the patients who had dose interruption, 59% experienced recurrence of rash upon reintroduction of ERLEADA®.
Hypothyroidism — In two randomized studies hypothyroidism, was reported for 8% of patients treated with ERLEADA® and 2% of patients treated with placebo based on assessments of thyroid-stimulating hormone (TSH) every 4 months. Elevated TSH occurred in 25% of patients treated with ERLEADA® and 7% of patients treated with placebo. The median onset was at the first scheduled assessment. There were no Grade 3 or 4 adverse reactions. Thyroid replacement therapy, when clinically indicated, should be initiated or dose-adjusted.
DRUG INTERACTIONS
Effect of Other Drugs on ERLEADA® — Co-administration of a strong CYP2C8 or CYP3A4 inhibitor is predicted to increase the steady-state exposure of the active moieties. No initial dose adjustment is necessary; however, reduce the ERLEADA® dose based on tolerability [see Dosage and Administration (2.2)].
Effect of ERLEADA® on Other Drugs — ERLEADA® is a strong inducer of CYP3A4 and CYP2C19, and a weak inducer of CYP2C9 in humans. Concomitant use of ERLEADA® with medications that are primarily metabolized by CYP3A4, CYP2C19, or CYP2C9 can result in lower exposure to these medications. Substitution for these medications is recommended when possible or evaluate for loss of activity if medication is continued. Concomitant administration of ERLEADA® with medications that are substrates of UDP-glucuronosyl transferase (UGT) can result in decreased exposure. Use caution if substrates of UGT must be co-administered with ERLEADA® and evaluate for loss of activity.
P-gp, BCRP or OATP1B1 substrates — Apalutamide is a weak inducer of P-glycoprotein (P-gp), breast cancer resistance protein (BCRP), and organic anion transporting polypeptide 1B1 (OATP1B1) clinically. Concomitant use of ERLEADA® with medications that are substrates of P-gp, BCRP, or OATP1B1 can result in lower exposure of these medications. Use caution if substrates of P-gp, BCRP or OATP1B1 must be co-administered with ERLEADA® and evaluate for loss of activity if medication is continued.
Please see the full Prescribing Information for ERLEADA®.
About the Janssen Pharmaceutical Companies of Johnson & Johnson
At Janssen, we’re creating a future where disease is a thing of the past. We’re the Pharmaceutical Companies of Johnson & Johnson, working tirelessly to make that future a reality for patients everywhere by fighting sickness with science, improving access with ingenuity, and healing hopelessness with heart. We focus on areas of medicine where we can make the biggest difference: Cardiovascular & Metabolism, Immunology, Infectious Diseases & Vaccines, Neuroscience, Oncology, and Pulmonary Hypertension.
Learn more at www.janssen.com. Follow us at www.twitter.com/JanssenGlobal. Janssen Research & Development, LLC and Janssen Biotech, Inc. are part of the Janssen Pharmaceutical Companies of Johnson & Johnson.
Cautions Concerning Forward-Looking Statements
This press release contains "forward-looking statements" as defined in the Private Securities Litigation Reform Act of 1995 regarding ERLEADA® (apalutamide). The reader is cautioned not to rely on these forward-looking statements. These statements are based on current expectations of future events. If underlying assumptions prove inaccurate or known or unknown risks or uncertainties materialize, actual results could vary materially from the expectations and projections of Janssen Research & Development, LLC, any of the other Janssen Pharmaceutical Companies and/or Johnson & Johnson. Risks and uncertainties include, but are not limited to: challenges and uncertainties inherent in product research and development, including the uncertainty of clinical success and of obtaining regulatory approvals; uncertainty of commercial success; manufacturing difficulties and delays; competition, including technological advances, new products and patents attained by competitors; challenges to patents; product efficacy or safety concerns resulting in product recalls or regulatory action; changes in behavior and spending patterns of purchasers of health care products and services; changes to applicable laws and regulations, including global health care reforms; and trends toward health care cost containment. A further list and descriptions of these risks, uncertainties and other factors can be found in Johnson & Johnson's Annual Report on Form 10-K for the fiscal year ended December 30, 2018, including in the sections captioned “Cautionary Note Regarding Forward-Looking Statements” and “Item 1A. Risk Factors,” and in the company’s most recently filed Quarterly Report on Form 10-Q, and the company’s subsequent filings with the Securities and Exchange Commission. Copies of these filings are available online at www.sec.gov, www.jnj.com or on request from Johnson & Johnson. Neither the Janssen Pharmaceutical Companies of Johnson & Johnson nor Johnson & Johnson undertakes to update any forward-looking statement as a result of new information or future events or developments.
Media Inquiries:
Michelle Larkin
Phone: 1-610-304-5842
Suzanne Frost
Phone: 1-416-317-0304
Investor Relations:
Christopher DelOrefice
Phone: 1-732-524-2955
Lesley Fishman
Phone: 1-732-524-3922
U.S. Medical Inquiries:
1-800-526-7736
1 ERLEADA® Prescribing Information, September 17, 2019.
2 Supplement: Scher HI, Solo K, Valant J, Todd MB, Mehra M et al. Prevalence of Prostate Cancer Clinical States and Mortality in the United States: Estimates Using a Dynamic Progression Model. PLoS One. 2015; 10(10): 1-2.
3 Chi, K. Apalutamide for Metastatic, Castration Sensitive Prostate Cancer. New England Journal of Medicine. Accessed September 2019.
4 American Society of Clinical Oncology. ASCO Answers: Prostate Cancer (2018). http://www.cancer.net/sites/cancer.net/files/asco_answers_guide_prostate.pdf. Accessed September 2019.
5 NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for Prostate Cancer V.4.2019. National Comprehensive Cancer Network, Inc. 2019. All rights reserved. Updated August 2019.
6 American Urological Association. Castration-Resistant Prostate Cancer Guidelines. http://www.auanet.org/guidelines/castration-resistant-prostate-cancer-(2013-amended-2018). Accessed September 2019.