Express Scripts Saved Plans $45 Billion on Prescription Drugs in 2018
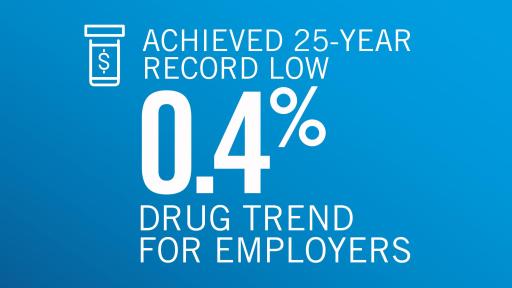
- -- Delivered a record low 0.4 percent drug trend across employer-sponsored plans
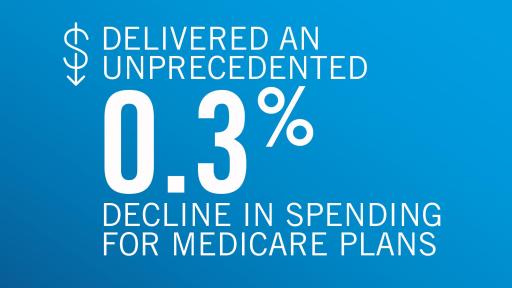
- -- Reduced per-beneficiary drug spending by 0.3 percent across Medicare plans
- -- Decreased unit drug costs for employer, Medicare and health exchange plans
- -- Expanded access to innovative medications through solutions that improve quality and affordability
ST. LOUIS, February 6, 2019 — Express Scripts clinical innovations saved its clients $45 billion in 2018 and delivered a 25-year record low drug trend of just 0.4 percent across employer-sponsored plans, according to data released today in its annual Drug Trend Report, an authoritative analysis of drug spending in the U.S.
Express Scripts’ solutions for driving lower drug prices and fostering the use of lower-net-cost treatments are making medication more accessible for beneficiaries. Unit drug costs decreased in 2018 for employer-sponsored and Medicare plans, while utilization of medications rose.
Patients in employer-sponsored plans paid just 6 cents more, on average, for a 30-day prescription than in 2017. Out-of-pocket costs, inclusive of deductibles and prescription drug copayments, for members of employer-sponsored plans were 15 percent of total prescription costs in 2018.
“We are creating a sustainable future for plan sponsors while improving access for patients,” said Glen Stettin, M.D., Senior Vice President and Chief Innovation Officer, Express Scripts. “By ensuring people get the right medicine at the right time at the right cost, Express Scripts helped tens of millions of people get the most value for each dollar spent on prescription drugs; helped reduce annual drug spending for 50 percent of its employer-sponsored plans, and achieved an unprecedented 0.3 percent decrease in drug spending for Medicare plans in 2018.”
While overall drug spending across employer-sponsored plans rose just 0.4 percent, spending on traditional, non-specialty medications decreased 5.8 percent. Spending on specialty medications increased 9.4 percent, down 1.9 percent from 2017. Of note:
- Specialty medications now account for 44.7 percent of total drug spending, up 3.9 percent from 2017.
- The inflammatory conditions therapy class, which includes therapies to treat conditions such as rheumatoid arthritis and Crohn’s disease, was the costliest therapy class for the third consecutive year, costing employers $174.45 per member per year in 2018, up 14 percent from 2017.
- Diabetes was the second costliest therapy class for employers at $114.85 per member per year, an increase of 4.1 percent over 2017. Spending on insulin, which accounts for 15.3 percent of diabetes prescriptions, increased just 0.3 percent in 2018, with a 1.5 percent decline in unit costs and a 1.8 percent rise in utilization. In 2018, patients paid 16.9 percent of total insulin costs, an average of $43.19 per prescription, up $3.33 from 2017.
NEW @ExpressScripts report shows value-based programs, discounted #drugprices and greater use of lower-cost drugs led to lowest annual drug spending in 25 years https://my.express-scripts.com/2018reports.html Tweet
Tweets by ExpressScripts
Express Scripts SafeGuardRx® Leads the Way in Value-Based Care
Plans enrolled in SafeGuardRx programs, which closely manage high-cost drug classes, experienced better trends in the targeted therapy classes than plans not enrolled. For example:
- Plans enrolled in the Diabetes Care ValueSM program had a 4.3 percent decrease in spending for diabetes medications, compared with a 7.5 percent increase in spending for plans not enrolled.
- Since 2014, the Hepatitis Cure Value® program has improved the affordability and accessibility of hepatitis C therapies, provided care by specialist pharmacists to ensure therapy completion and delivered a 96 percent cure rate. As a result of these efforts, spending on hepatitis C therapies declined nearly 48 percent in 2018, which kept the therapy class out of the top 15 costliest therapy classes for the first time since 2013.
“Looking ahead to 2019 and beyond, we’re doubling down on our focus on better outcomes and making care more personal and better connected across the care continuum. While these have been tenets of our work for decades, they will become even more important as we look to provide simpler, more affordable access for our members,” Dr. Stettin said.
Price Inflation
Despite list price inflation of 7.3 percent for the most commonly used traditional brand medications in 2018, drug costs for traditional drugs declined 6.5 percent for Express Scripts’ employer-sponsored plans, 5.5 percent for Medicare plans and 5.6 percent for exchange plans.
New in the 2018 report, the Express Scripts Specialty Prescription Price Index added tracking of list price inflation and deflation for the most commonly used specialty medications in addition to traditional medications. While list prices for brand-name specialty drugs increased 7.1 percent in 2018, specialty drug costs increased only 2.1 percent for our employer-sponsored plans, 2.4 percent for Medicare plans, and 2 percent for exchange plans.
Over the past five years, list prices for traditional brand medications have increased 62 percent; list prices for specialty brand medications have increased 57 percent. Prices for the most commonly used traditional generics have decreased 36.9 percent; prices for the most commonly used specialty generics have decreased 20 percent.
Forecast
Express Scripts forecasts drug spending per beneficiary to increase by 2 percent, on average, annually through 2021.
“We made great progress in 2018, but there is more work to be done, particularly for members who are still exposed to high out-of-pocket costs,” Dr. Stettin said. “From expanding the discounts available in our InsideRx® prescription savings program, which saved $400 million for uninsured and underinsured consumers since the program began in May 2017, to providing new digital resources that direct members to lowest-cost therapies, to advocating for smarter public policies, we are leading the way to make care better and more affordable for everyone we serve.”
In a companion report that reviews drug spending trends and public policy, Express Scripts once again calls upon stakeholders to act on a prescription drug affordability agenda by passing and signing the Creating and Restoring Equal Access to Equivalent Samples (CREATES) Act, supporting legislation to prohibit “pay-for-delay” arrangements, supporting use of electronic prescribing for controlled substances in public programs, and unleashing the potential of value-based benefit designs. This agenda builds upon our legislative success championing recommendations in the Express Scripts 2018 Prescription Drug Pricing Public Policy Analysis, including mandates for electronic prior authorization in Medicare, legislation on so-called “pharmacy gag clauses,” and laws requiring pharmaceutical companies to disclose patent settlements.
About the 2018 Express Scripts Drug Trend Report
Our annual Drug Trend Report is among the industry’s most comprehensive analysis of annual changes in the cost and use of prescription medications in the U.S. The research examined the de-identified prescription drug use data of approximately 34.2 million people with a pharmacy benefit plan administered by Express Scripts, including those in an employer-sponsored, Medicare, Medicaid or health insurance exchange plan.
To access the report, please visit http://lab.express-scripts.com/lab/drug-trend-report.
About Express Scripts
Express Scripts is a health care opportunity company. Empowered by our legacy as an industry innovator, we dare to imagine — and deliver — a better health care system with greater choice, predictability, affordability and improved outcomes. From pharmacy and medical benefits management, to specialty pharmacy care and everything in between, we uncover opportunities to make health care better.
We stand alongside our clients and partners, collaborating to develop personalized solutions that make a meaningful difference in the lives of those we serve, whenever and wherever it’s needed. We believe health care can do more.
We are Champions For BetterSM.
Express Scripts, part of Cigna Corporation, unlocks new value in pharmacy, medical, and beyond to further total health for all.
Media Contact:
Jennifer Luddy
(201) 269-6402
[email protected]